Internal NETEC document confirms H5N1 avian influenza preparedness at the core mission of new taxpayer funded hospital network.

The U.S. Department of Health and Human Services (HHS), through its Administration for Strategic Preparedness and Response (ASPR), is funding a $37.5 million national hospital expansion to prepare for H5N1 bird flu and other high-consequence pathogens, according to a newly released internal federal document issued by the National Emerging Special Pathogens Training and Education Center (NETEC).
NIH and NIAID—which are under HHS, led by Secretary Robert F. Kennedy Jr.—are funding experiments that create brand new bird flu pathogens, raising conflict of interest worries as well as questions about the government’s motives (see list of articles below this article detailing these many experiments).
NIAID chief Dr. Jeffery Taubenberger is directing U.S. tax dollars toward bird flu reverse genetics experiments while holding a patent for the carcinogenic BPL-based bird flu jab at the center of the Trump administration’s $500 million ‘Generation Gold Standard’ program—funding both the problem and the patented solution.
The new document—an internal Request for Proposal (RFP) dated October 15, 2025—details how HHS will use NETEC, a consortium of Emory University, the University of Nebraska Medical Center, and NYC Health + Hospitals/Bellevue, to distribute federal funds to 75 hospitals across the United States, converting them into federally designated “Level 2 Special Pathogen Treatment Centers” (SPTCs).
Each facility is eligible to receive $500,000 under the ASPR-funded NSPS Level 2 Special Pathogen Treatment and Network Development (STAND) Award.
The RFP’s stated purpose is to “accelerate the domestic health care system’s readiness for [high-consequence infectious diseases], such as H5N1, Ebola, and others.”
Per the document:
“Under the guidance of ASPR, NETEC is now awarding $37,500,000 in funding to 75 facilities ($500,000 per facility) as they work to meet the requirements of NSPS Level 2 facilities. The funding will support activities such as training health care personnel, upgrading infrastructure, and acquiring specialized equipment to ensure Level 2 facilities meet NSPS minimum capabilities. These efforts are expected to ultimately result in the verification of funded facilities as Level 2 SPTCs. This expansion significantly enhances the nation’s surge capacity and geographic reach for managing HCIDs.”
The move comes as governments all over the world say they are creating hybrid bird flu viruses in biolabs, raising national security fears of another pandemic, whether intentional or accidental.
Those same countries ramp up bird flu vaccine production and distribution.
Meaning, once again, governments are creating both the problem and “solution” to another pandemic, raising conflict-of-interest worries.
Congress, the White House, the Department of Energy, the FBI, the CIA, and Germany’s Federal Intelligence Service (BND) have confirmed that the COVID-19 pandemic was likely the result of lab-engineered pathogen manipulation.
H5N1 Avian Influenza Explicitly Listed as a Federal Priority
While the public press release announcing the grant avoided mentioning bird flu, the internal NETEC RFP directly names H5N1 avian influenza as a top threat driving the new hospital buildout.
“The emergence and sustained transmission of HCIDs, such as Ebola, mpox, and avian influenza (H5N1), have overwhelmed hospitals, exhausted critical resources, and underscored the necessity for coordinated efforts to protect health care workers while ensuring the delivery of safe and effective patient care.”
This wording makes clear that H5N1 preparedness—not just general infectious disease readiness—is a central justification for the $37.5 million initiative.
Federal Pandemic Infrastructure Expansion
Under ASPR’s direction, NETEC will administer the new program as part of the National Special Pathogen System (NSPS)—a tiered national network of pathogen treatment centers first created after the 2014–2016 Ebola outbreak.
The new Level 2 centers are described as “the backbone of a resilient, skilled response to special pathogen threats,” designed to serve as regional treatment hubs capable of handling clusters of patients during future high-consequence disease outbreaks.
The funding will support:
- Upgrading isolation infrastructure,
- Purchasing specialized containment equipment,
- Training staff in special pathogen protocols, and
- Coordinating with existing Level 1 Regional Emerging Special Pathogen Treatment Centers (RESPTCs).
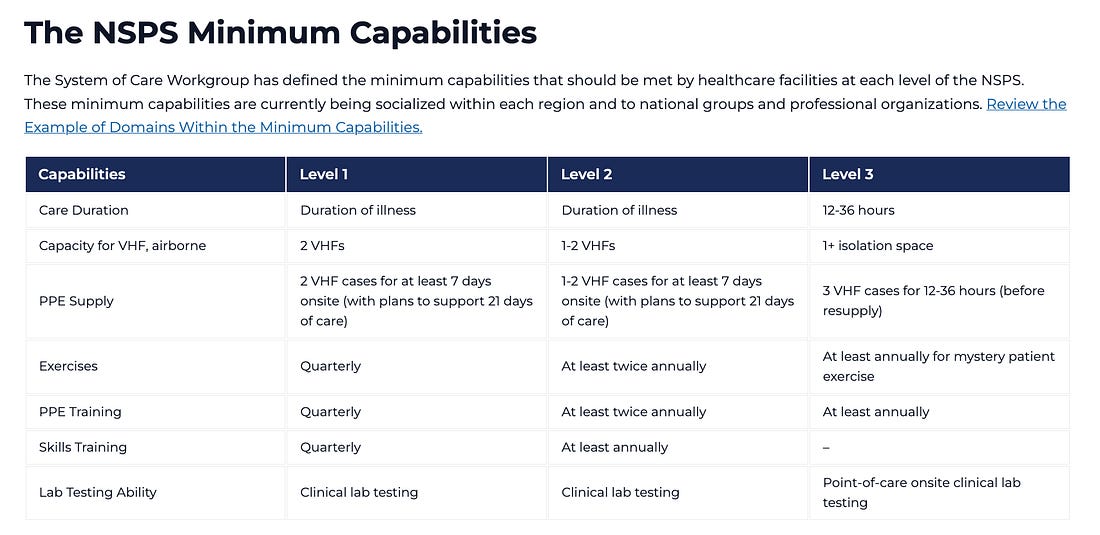
Awardees must demonstrate “substantial progress towards meeting the minimum capabilities of a Level 2 NSPS facility” by the end of the funding period.
‘Level 2’ Centers Will Treat Patients for the Duration of Illness
Each Level 2 facility, the RFP explains, must have “the capacity to deliver specialized care to clusters of patients suspected of or infected by a special pathogen” and “serve as the primary patient care delivery center.”
Notably, funded hospitals must also agree to:
“Serve as regional and national assets and accept patients from outside of the United States or outside their respective state, county, or local jurisdiction if requested.”
That clause effectively integrates participating hospitals into the federal pandemic command structure under ASPR oversight, expanding the U.S. government’s ability to move special pathogen cases across state or national lines.
Institutionalization of Permanent Biosecurity Infrastructure
The NETEC RFP uses unmistakable national security language, describing high-consequence infectious diseases (HCIDs) as threats to “the nation’s health, economy, and national security.”
It emphasizes what it characterizes as the need for “enhanced biosecurity frameworks, robust clinical readiness, and surge capacity across hospitals,” positioning the Level 2 expansion as a cornerstone of HHS’s long-term pandemic preparedness architecture.
The RFP even notes that NETEC “has demonstrated its critical role in strengthening national health security by coordinating National Special Pathogen System responses to novel respiratory pathogens, mpox, and Lassa fever.”
In other words, the federal government is now formally embedding outbreak containment systems inside civilian hospitals, justified by avian influenza and other potential zoonotic spillover threats.
Timeline & Implementation
Applications for the NSPS Level 2 STAND Award opened October 15, 2025, and close December 2, 2025.
Final selections are expected by January 5, 2026, with the official “period of performance” scheduled from January 5 through June 29, 2026.
Eligible applicants must have:
- An onsite emergency department,
- Airborne infection isolation rooms,
- Critical care and inpatient capacity, and
- A sufficient baseline of resources to achieve Level 2 verification.
The RFP explicitly prohibits use of the funds for direct clinical care or research—focusing instead on infrastructure, staff training, and equipment acquisition.
From COVID Lessons to Bird Flu Systems
NETEC was originally established in 2015 after the U.S. treated imported Ebola cases.
During the COVID-19 pandemic, it served as a national training and coordination body for pathogen response across hospitals.
Now, under ASPR’s expanded authority, NETEC’s mission has evolved from temporary outbreak response to permanent pandemic infrastructure building, with H5N1 preparedness front and center.
The RFP states that the expansion “significantly enhances the nation’s surge capacity and geographic reach for managing HCIDs,” embedding what amounts to federally funded containment capacity across the entire U.S. hospital network.
Bottom Line
The internal NETEC document reveals that HHS’s Administration for Strategic Preparedness and Response (ASPR) is quietly constructing a nationwide bird flu hospital network under the banner of “special pathogen preparedness.”
The $37.5 million program explicitly cites H5N1 avian influenza as a primary threat and converts 75 hospitals into federally integrated treatment hubs for future high-risk pathogen outbreaks.
This marks yet another major escalation in the institutionalization of permanent pandemic infrastructure inside the United States, built through administrative expansion under the HHS biosecurity apparatus.


Leave a comment